When can you enroll in Medicare?
When you first get Medicare (Initial Enrollment Periods for Part C & Part D)
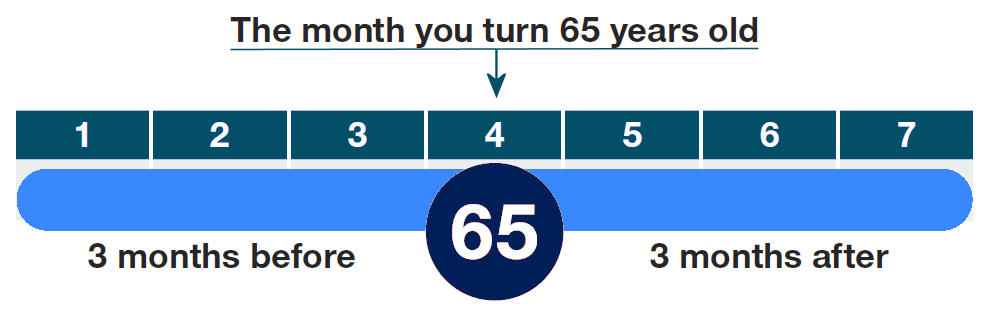
Most people enroll during their Initial Enrollment Period (IEP) which begins three months before the month of your 65th birthday, and ends three months after. In most cases Part A and Part B are effective in the first day of your birth month. Other enrollment periods are listed below.
- I am newly eligible for Medicare because I have a disability (under 65).
- I am already eligible for Medicare because of a disability, and I turned 65.
- I do not have Medicare Part A coverage, and I enrolled in Medicare Part B during the Part B General Enrollment Period (January 1–March 31).
- I have Medicare Part A coverage, and I enrolled in Medicare Part B during the Part B General Enrollment Period (January 1–March 31).
- During certain times each year (yearly enrollment periods for Part C & Part D)
When Can I Change Plans?
Annual Open Enrollment Period (AEP) – October 15 through December 7
What you can do during AEP:
- Change from Original Medicare to a Medicare Advantage Plan.
- Change from a Medicare Advantage Plan back to Original Medicare.
- Switch from one Medicare Advantage Plan to another Medicare Advantage Plan.
- Switch from a Medicare Advantage Plan that doesn’t offer drug coverage to a Medicare Advantage Plan that offers drug coverage.
- Switch from a Medicare Advantage Plan that offers drug coverage to a
- Medicare Advantage Plan that doesn’t offer drug coverage.
- Join a Medicare Prescription Drug Plan.
- Switch from one Medicare drug plan to another Medicare drug plan.
- Drop your Medicare prescription drug coverage completely.
Medicare Advantage Open Enrollment Period – January 1 through March 31
What you can do during MA-OEP:
- If you’re in a Medicare Advantage Plan (with or without drug coverage), you can switch to another Medicare Advantage Plan (with or without drug coverage).
- You can dis-enroll from your Medicare Advantage Plan and return to Original Medicare. If you choose to do so, you’ll be able to join a Medicare Prescription Drug Plan.
- If you enrolled in a Medicare Advantage Plan during your Initial Enrollment Period, you can change to another Medicare Advantage Plan (with or without drug coverage) or go back to Original Medicare (with or without drug coverage) within the first 3 months you have Medicare.
What your can’t do during MA-OEP:
- Switch from Original Medicare to a Medicare Advantage Plan.
- Join a Medicare Prescription Drug Plan if you’re in Original Medicare.
- Switch from one Medicare Prescription Drug Plan to another if you’re in Original Medicare.
Special Enrollment Periods
You can make changes to your Medicare Advantage and Medicare prescription drug coverage when certain events happen in your life, like if you move or you lose other insurance coverage. These chances to make changes are called Special Enrollment Periods (SEPs). Rules about when you can make changes and the type of changes you can make are different for each SEP.
- You change where you live
- I moved to a new address that isn’t in my plan’s service area.
- I moved to a new address that’s still in my plan’s service area, but I have new plan options in my new location.
- I moved back to the U.S. after living outside the country.
- I just moved into, currently live in, or just moved out of an institution (like a skilled nursing facility or long-term care hospital).
- I’m released from jail.
You lose your current coverage
- I’m no longer eligible for Medicaid.
- I left coverage from my employer or union (including COBRA coverage).
- I involuntarily lose other drug coverage that’s as good as Medicare drug coverage (creditable coverage), or my other coverage changes and is no longer creditable.
- I had drug coverage through a Medicare Cost Plan and I left the plan.
- I dropped my coverage in a Program of All-inclusive Care for the Elderly (PACE) plan.
You have a chance to get other coverage
- I have a chance to enroll in other coverage offered by my employer or union.
- I have or am enrolling in other drug coverage as good as Medicare prescription drug coverage (like TRICARE or VA coverage).
- I enrolled in a Program of All-inclusive Care for the Elderly (PACE) plan.
- Your plan changes its contract with Medicare
- Medicare takes an official action (called a “sanction”) because of a problem with the plan that affects me.
- Medicare ends (terminates) my plan’s contract.
- My Medicare Advantage Plan, Medicare Prescription Drug Plan, or Medicare Cost Plan’s contract with Medicare isn’t renewed.
Other special situations
- I’m eligible for both Medicare and Medicaid.
- I qualify for Extra Help paying for Medicare prescription drug coverage.
- I’m enrolled in a State Pharmaceutical Assistance Program (SPAP) or lose SPAP eligibility.
- I dropped a Medigap policy the first time I joined a Medicare Advantage Plan.
- I have a severe or disabling condition, and there’s a Medicare Chronic Care Special Needs Plan (SNP) available that serves people with my condition.
- I’m enrolled in a Special Needs Plan (SNP) and no longer have a condition that qualifies as a special need that the plan serves.
- I joined a plan, or chose not to join a plan, due to an error by a federal employee.
- I wasn’t properly told that my other private drug coverage wasn’t as good as Medicare drug coverage (creditable coverage).
- I wasn’t properly told that I was losing private drug coverage that was as good as Medicare drug coverage (creditable coverage).
